another positive step towards legally using psilocybin to alleviate intractable clinical depressions ...
The big idea: should doctors be able to prescribe psychedelics? | Drugs | The Guardian
The big idea: should doctors be able to prescribe psychedelics?
A move to allow Australian psychiatrists to treat depression with psilocybin may herald a new era
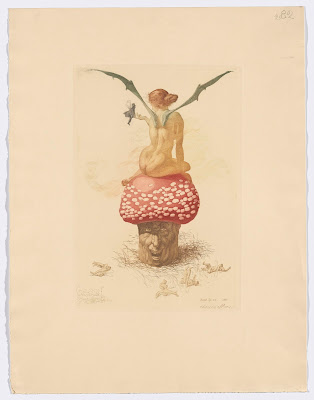
So-called magic mushrooms (those that contain the molecule psilocybin) have been used by people around the world medicinally and ceremonially for a very long time. Rock art in Kimberley, Western Australia, that depicts mushroom-headed beings, suggests people were using them 10,000 years ago to attain trance-like states. Strikingly similar images have been found in the Sandawe paintings of eastern Tanzania and in the Algerian Sahara. Now, after decades of these hallucinogenic fungi being consigned to the grubby margins of legality, humans appear to be rediscovering their benefits.
From July, authorised psychiatrists in Australia will be permitted to prescribe psilocybin to patients with treatment-resistant depression. This hasn’t come out of the blue: the drug is a major ingredient in what has been dubbed the psychedelic renaissance – a resurgence of public interest and research in substances that began to be recognised for their medicinal qualities in the 1950s, before a wave of moral panic and irrational legislation placed them off-limits for years.
For the patients in Australia who will be offered the treatment, there will be few other therapeutic options that stand a chance of alleviating their desperate suffering. Traditional antidepressants, even when they work, have a slow onset, can come with significant negative side effects and may need to be taken daily for years. Several clinical trials have now shown that two doses of psilocybin in the right setting, with appropriate supportive talking therapy, appears to offer a low-risk, effective and tolerable treatment for depression that lasts for weeks or months with very little downside. The studies may be small and imperfect so far – there are bigger trials in the pipeline – but the initial results are encouraging.
Interest in the therapeutic effects of psychedelic drugs such as psilocybin has – if you’ll forgive the pun – mushroomed over the last 15 years. In 2021, investment in the psychedelic sector reached almost $2bn. There are hundreds of registered clinical trials exploring the effects of psychedelics on a range of conditions. But in order to be able to use them as safely as possible, there is still a lot we need to learn about these powerful psychoactive drugs – for example, how they interact with other medications. Many clinical trials also don’t tend to follow up on patients for very long after treatment. Much work has yet to be done, but researchers and clinicians are hampered by the archaic and misguided legal classification of psychedelics.
It’s important to keep things in perspective. Something about psychedelics induces a kind of evangelical fervour.
In the UK, magic mushrooms are still categorised as class A drugs, incongruously rubbing shoulders with extremely harmful substances such as crack cocaine and heroin. As such, possession alone can carry a prison sentence of up to seven years. To acquire them for legitimate research purposes is an expensive and heavily bureaucratic process.
The decision in Australia to allow psychiatrists to prescribe this drug is both forward-thinking and pragmatic. Psychedelics are likely to eventually become mainstream in our society one way or another, under the pressure of both mounting medical evidence and the juggernaut of capital. The issue is how we want them to arrive: surfing on a bubble of hype, flogged at a premium by wellness gurus with no qualifications? Or, as Australia has decided, initially in a clinical setting with well-established ethical frameworks and long-term follow-up, supervised by practitioners with the knowledge and experience to handle unexpected or adverse outcomes?
It’s important to keep things in perspective. There is something about psychedelics that induces a kind of evangelical fervour among some proponents. They are heralded as a panacea. It’s unsurprising, perhaps, given the lack of innovation in psychiatric treatments over the last 50 years and the huge burden of mental illness with which society currently struggles. Drugs like psilocybin do indeed have some remarkable effects: they appear to help people to get out of a mental rut, interrupting patterns of repetitive harmful mental behaviour in which they have long been stuck.
But they are not a magic bullet and, rarely, can cause harm – especially if users are at a higher risk of psychotic illness. Even for those unlikely to develop a clinically significant problem from using psychedelics, they are not to be trifled with. The waking dream-like state that they can induce, loaded with symbolism and strange imagery, has the potential to be a profound and sometimes shattering experience, even if the “trip” is not a bad one. But with expert guidance and support, even a challenging experience can become psychologically useful. Psilocybin has the capacity to create a state of vulnerability, laying open the heart and mind. It requires scrupulous ethical conduct on the part of providers in order to avoid exploitation.
Introducing more widespread use of psychedelics in a sober, scientifically informed and ethically rigorous way minimises the risk of history repeating itself with a stifling backlash that could foreclose their potential usefulness in tackling the mental health crisis. Some may want to see restrictions on substances loosened beyond strictly medical settings, but as a society we have to start somewhere. While British psychiatry has not been without its own serious problems in the past, it is now the best place for us to start any opening up, with its well-developed safeguards and the obligation to record events.
With time, we may need to go further still. The cases of misery, pain and mental suffering that make it to the GP’s surgery, let alone a mental health specialist, are the tip of the iceberg. Perhaps one day drugs like psilocybin will reach further into communities, with people enabled and empowered to use them safely and effectively via a pharmacy, without the need for a prescription. Not every ailment needs a doctor, after all. For now we would do well to follow in Australia’s footsteps: open the clinic door to magic mushrooms, and politely invite them in.


Comments
Post a Comment